Do You Have a Herniated Disk? Symptoms, Diagnosis & Treatments
 A herniated disk, or a slipped disk, is by far the most common cause of neck pain, lower back pain, and nerve-related leg pain. Herniated disks have a high prevalence among adults aged 35 and older, with various causes ranging from repetitive injuries to sudden strain, other illnesses, and weight gain. Sudden pain near the back and shoulder, neck pain, neck spasms, weakness or tingling in the legs, or pain radiating through the buttocks often points at a herniated disk at one or several points in the spine.
A herniated disk, or a slipped disk, is by far the most common cause of neck pain, lower back pain, and nerve-related leg pain. Herniated disks have a high prevalence among adults aged 35 and older, with various causes ranging from repetitive injuries to sudden strain, other illnesses, and weight gain. Sudden pain near the back and shoulder, neck pain, neck spasms, weakness or tingling in the legs, or pain radiating through the buttocks often points at a herniated disk at one or several points in the spine.
However, these symptoms are not exclusively caused by disk problems. Despite its prevalence, doctors go to certain lengths to identify the cause of their patient’s pain. Before we get into how herniated disks are identified, let us explore how they occur.
What Is a Herniated Disk?
The spine consists of a column of bones called vertebrae, each one separated by a spinal disk. Spinal disks are soft in the center (the nucleus pulposus) and rubbery on the outside (the annulus fibrosus). These disks act as shock absorbers and connective tissue between the bones while enabling the spine to flex within a certain range of motion. They are tough but can only withstand so much punishment over the years.
Through enough wear-and-tear, these disks become weaker, raising the risk of a potential tear, swelling, or herniation. When a spinal disk is herniated, some of its soft-core spills out of its rubbery shell. This in and of itself does not cause much pain – but it can lead to nerve compression, as the contents of the disk press on the nerve roots that connect the nerves innervating our body to the spinal cord, and thus, the brain.
Depending on what disk is affected, the compression can occur at different spine points, causing pain, numbing, weakness, and tingling in different parts of the body. By far, the most common location for a herniated disk is in the lower back, near the roots of the sciatic nerve. The second most common location is the neck. Finally, only a small percentage of disk herniations occur in the thoracic (upper back) region.
Signs and Symptoms of a Herniated Disk
The most common sign of a herniated disk is pain – specifically, pain originating in one leg, the back, or neck, accompanied by signs of weakness or numbing. However, it is important to note that a herniated disk is not the only cause of these symptoms. A few other symptoms to keep an eye on include:
For herniation in the lower back:
-
- Pain in one leg and buttock.
- Tingling in the feet or legs.
- Weakness in the legs.
For herniation in the neck:
-
- Pain near or above the shoulder blade.
- Muscle spasms in the neck.
- Pain radiating into the arm.
- Neck pain.
It should also be noted that a herniated disk or a slipped disk might not have any symptoms and may be caught by a doctor during a routine checkup without pain or numbness. This is because the herniation does not necessarily need to affect the nerves, depending on its size and severity. Instead, the symptoms start once the disk contents have advanced enough to compress the nerves in and around the spine.
How Is a Slipped Disk Diagnosed?
The diagnostic process begins with a physical exam to narrow down the source of the pain. Next, doctors will be testing for nerve function (through an electromyogram, testing strength) and discomfort. They will also ask about your medical history (to help provide important context for your symptoms) and ask you to recall when and where the pain or discomfort started and what made it worse.
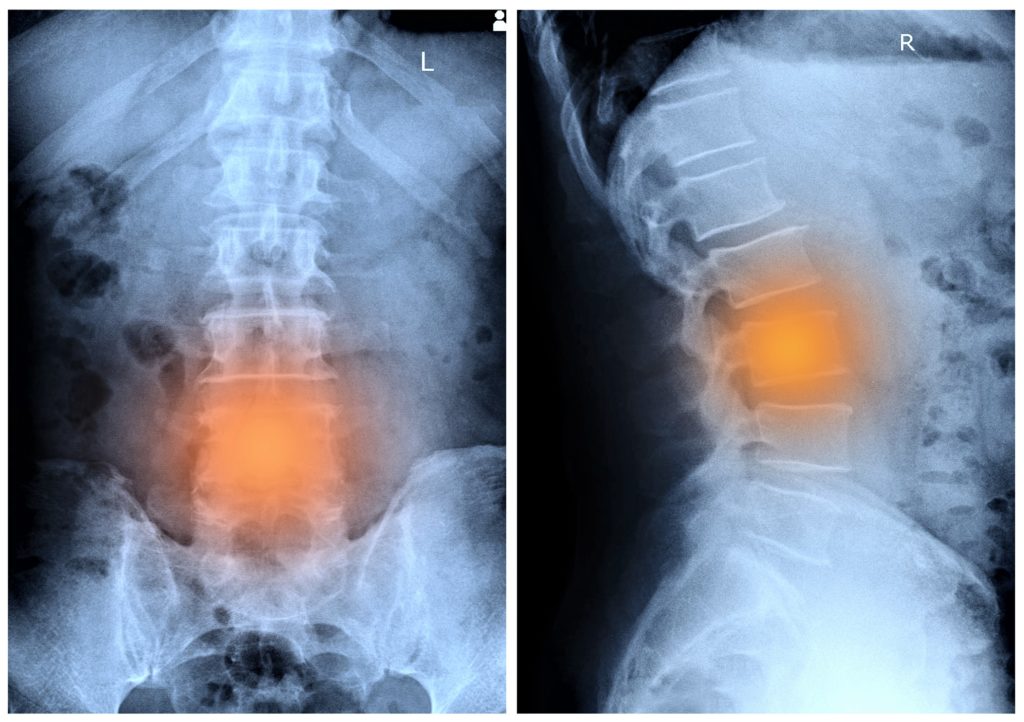
The main course in the diagnostic process for a herniated disk is an imaging test. Once doctors have an idea of what they should be looking for, they can order tests to identify if the region the pain is linked to is being affected by a herniated disk. Such tests include fluoroscopy, x-rays, CT scanning, or an MRI test.
How Do Herniated Disks Occur?
Perhaps the largest factor behind a herniated disk is age. But, by and large, human aging is still irreversible – and our spinal disks are one of those body parts that do not necessarily stand the test of time, especially over decades of use. In addition, certain activities and events drastically speed up the process (excessive bodyweight, manual labor, smoking).
Others can act as a preventative measure for disk herniation (core strength, healthy diet) and other disk complications. Disk herniation can occur suddenly (from bending down to pick something up, twisting around, a golf swing, lifting furniture), and often because of accumulated wear-and-tear.
Sometimes, a disk is herniated without any symptoms, and it’s only once things get worse than the pain starts to set in. Herniated disks are not exclusive to adults aged 35 and older. Disk herniation can occur at any age. In children, disk herniations are often the result of congenital spine malformations.
Herniated Disk Complications
Pain alone is not the only problem associated with a herniated disk. While conservative therapies – such as pain management, rest, and exercise – are often enough to treat a herniated disk in a few weeks, ignoring the problem or piling onto your injury can result in severe consequences, including cauda equina syndrome (inability to control bowel movements and eventual paralysis). In addition, chronic back, leg, or neck pain may also begin with an untreated herniated disk.
Treating a Slipped Disk
The body does most of the legwork when treating a herniated disk. Therefore, treatment consists of simply aiding the body and reducing pain. Bed rest, while helpful at first, is not encouraged for long periods of time. Instead, the treatment process may include some degree of physical therapy and occupational therapy to build core strength and improve posture in the patient’s day-to-day life.
Medication for a herniated disk may range from anti-inflammation drugs to targeted spinal injections. In severe cases, surgery may be an option to help address the pressure on the nerve, especially in recurring or chronic cases. Prevention is another critical component of the treatment process.
But, again, physical exercise is the most valuable tool, in this case, building the patient’s total core musculature (not just the visible abdominal muscles, but all the muscles surrounding and supporting the spine). Low-impact aerobic exercise and dietary changes also play a role in the treatment process, especially if the patient does not eat well or struggles with circulatory issues, compounding the risk of spinal injuries and slowing the healing process.
