Vertebroplasty Procedure, Recovery Time + More
 What does a vertebroplasty procedure look like? It is a non-invasive surgical procedure resulting in a stable spine structure. Read below to learn more.
What does a vertebroplasty procedure look like? It is a non-invasive surgical procedure resulting in a stable spine structure. Read below to learn more.
Spinal surgeries are crucial for treating illnesses, injuries, and conditions that threaten to deteriorate rapidly. Conservative treatments – such as rest, heat packs, and physical therapy – are not enough in cases where the spine itself may be physically compromised and where sudden complications could arise and put the patient at risk for permanent damage. However, surgeries don’t have to be invasive to work.
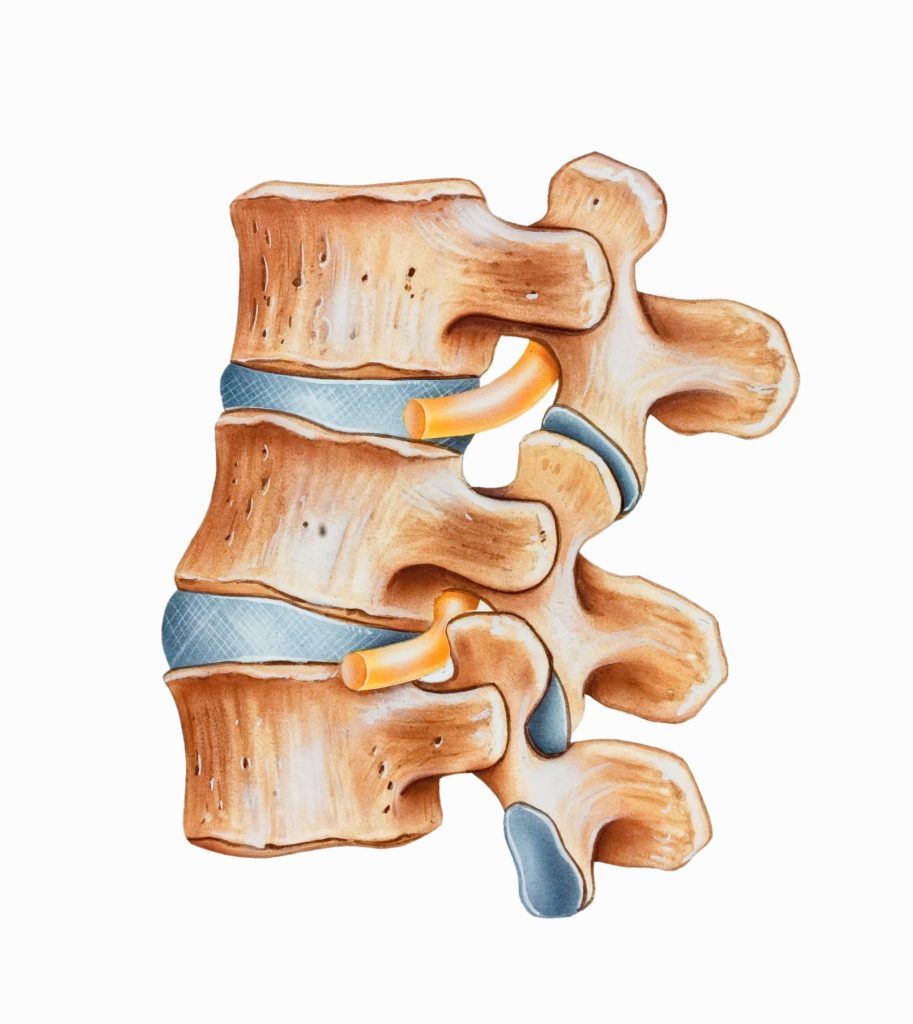
When a patient has fractured one or multiple vertebrae, surgery may be necessary to stabilize the bone and prevent further damage to the spinal cord and surrounding nerve roots. The procedure for stabilizing fractured vertebrae is called vertebroplasty.
What is Vertebroplasty?
Vertebroplasty is a non-invasive surgical procedure that involves injecting medical bone cement into the gaps and cracks of a vertebra that suffered a compression fracture, or VCF. The glue sets inside the bone and hardens, substituting bone tissue and stabilizing the vertebra.
The result is a stable structure in the spine. Because the cement solidifies and stabilizes the spine, the procedure can also reduce pain and swelling, or expedite the healing process in the area, reduce the likelihood of complications in the future, and reduce the patient’s reliance on pain medication.
There are generally two categories of medical bone cement used in vertebroplasty: calcium-based cement and acrylic cement. Modern operating rooms typically utilize calcium phosphate bone cement or polymethylmethacrylate (PMMA), also known as Plexiglass. Polymer-based bone cement dates back to the early 20th century and was especially popular in dental procedures before becoming integral to other arthroplasties.
Bone cement is also often used in knee, hip, and shoulder replacements, for implant fixation. Shortly before injection, bone cement is mixed (stored as two compounds, a powder, and a liquid) and begins to set soon after injection. Modern-day bone cement is sometimes also loaded with antibiotics to be used to treat infected joint arthroplasty.
Vertebroplasty vs. Kyphoplasty
Vertebroplasty and kyphoplasty are somewhat synonymous with one another. Kyphoplasty is just vertebroplasty with the additional use of a small balloon. This is designed to create space inside the vertebra and provide further structural support. The idea is that the balloon makes the space for the cement to fill and may be used to restore the height and structure of a person’s vertebra after it has been significantly damaged through a compression fracture.
For comparison’s sake, vertebroplasty itself wouldn’t magically add height to the bone – it would fill the gaps left by the fracture to avoid further damage. The use of a medical balloon helps minimally expand the bone during the procedure.
When is Vertebroplasty Applicable?
Vertebroplasty is usually reserved for vertebral compression fractures (VCF). These occur most often due to osteoporosis and age. Vertebral compression fractures are characterized by height loss, loss of flexibility in the back, and spinal deformation, as one or more vertebrae, are crushed or collapse inwards.
If a patient’s vertebra collapses unilaterally, which is often the case, a sharp angle may be created, causing kyphosis or a hunched back. This is because the front-facing part of the spinal bone compresses or crushes more commonly than the more structurally sound back portion of the bone, creating a slope. This forces the rest of the spine to lurch forward.
Osteoporosis is most frequent in post-menopausal women but can occur at any age and any sex. Certain lifestyle choices and genes increase the risk of a VCF, including strenuous labor, an overly sedentary lifestyle, obesity, and smoking. Other risk factors include low bone mineral density and rheumatoid arthritis. Cancer-related vertebral compression fractures may also require treatment in the form of vertebroplasty, depending on the circumstances of the patient’s case.
Not all patients who have experienced a vertebral compression fracture are a good candidate for vertebroplasty. Furthermore, not all good candidates for vertebroplasties are recognized.
VCFs continue to go underdiagnosed in men and are not always diagnosed in women. Many VCFs are asymptomatic, which generally means that they occur without causing pain. The height loss after a VCF can be relatively minimal and may go unnoticed for years.
However, if and when a VCF is diagnosed, there are still cases where certain factors serve to contraindicate vertebroplasty. These include:
- An allergy to the bone cement.
- An active infection in or around the area.
- Coagulation disorders (some of the medication used when performing the procedure may exacerbate the disorder and cause slowed healing and excessive bleeding).
- A stable fracture with no need for a VCF.
- Patients who have suffered no reduced quality of life or lack of mobility as a result of their fracture.
Vertebroplasty Procedure
The actual procedure for vertebroplasty is simple and usually does not require general anesthesia (unless the patient is in great pain and distress).
A local anesthetic may be applied via a guided syringe, followed by another for the cement mix. Imaging technology is used to guide the syringe into the fractured bone, either via fluoroscopy or ultrasound.
Recovery Time for a Vertebroplasty Procedure
After applying the injection, patients will be kept in observation. Because it is an entirely non-invasive and minor surgery, most patients can expect to recover within the day. Most hospitals discharge patients within the next 24 hours after vertebroplasty.
The typical recovery time for vertebroplasty is two hours spent under observation in a recovery room. If you experience any discomfort, the doctor may prescribe certain painkillers. The injection site should be kept dry for at least 24 hours. Some other things to keep in mind regarding post-op activities:
- Avoid heavy lifting and any strenuous activity.
- No driving for two weeks, depending on the severity of the condition.
- You may be given a back brace for further support.
Studies on the efficacy of vertebroplasty showed that a significant amount to the majority of patients (depending on the study) enjoyed reduced pain, reduced painkiller use, and increased mobility.
However, as mentioned previously, vertebroplasty (or kyphoplasty) is not always the ideal or only treatment for a VCF. Be sure to consult your doctor for other potential pain management options, as well as continued treatment if your pain lingers.
