What Aggravates Piriformis Syndrome?
Piriformis syndrome is a literal pain in the behind, yet despite its supposed prevalence, it is not well understood, nor is it properly documented in the general population. It is a “sciatica-like” condition, one characterized by symptoms that can often be mistaken for other conditions, yet one that also has unique characteristics and requires a specific and individualized treatment plan.
Piriformis syndrome is not a condition that can be immediately diagnosed. It occurs when the piriformis muscle swells and/or spasms, involuntarily and excessively contracting. The result is pain and discomfort in one buttock, and at times, sciatica pain symptoms triggered by the compression of the sciatic nerve running underneath the piriformis muscle.
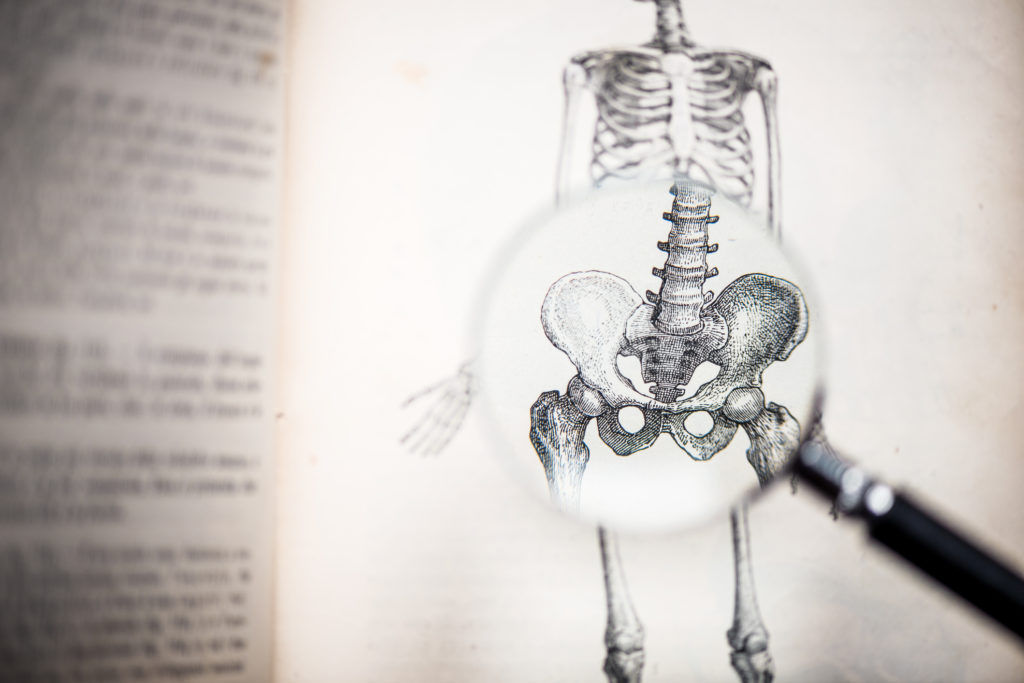
As a muscle, the piriformis is relatively small and located deep inside the buttocks, and it plays a minor role in the rotation of the hip and abduction of the leg. An injured or inflamed piriformis muscle can mimic the symptoms of sciatica, arthritis, bursitis, and different spinal conditions. Left untreated, piriformis syndrome can develop into other problems as a result of “compensatory movements” and maladaptation.
The affected leg is often weakened, range of motion and flexibility are worsened, and gait is changed, resulting in adaptations and pain along the entire posterior chain, leading to neck and head pain, lower back pain, and pain in various different seated and standing positions. Understanding what aggravates piriformis syndrome and managing it effectively and appropriately is important.
Diagnosing Piriformis Syndrome
Patients with piriformis syndrome will usually present with unilateral pain in the area, and may undergo a series of tests to determine piriformis syndrome and rule out other potential causes of pain, including disc degeneration/herniated discs, inflammation at some other point in the lower back or legs, sacroiliac joint dysfunction, a tumor, other causes of neurological pain, and more.
Your doctor may ask you to perform a series of stretches and movements to determine whether your mobility or strength has been impinged by a potential swollen or injured piriformis muscle, including the Freiberg test, the Pace test, and the Lasègue. Another common sign is external rotation in the only one foot (on the same side as the pain) while lying supine and totally relaxed, with pain exacerbated whenever the foot is brought to midline.
Different signs and symptoms may imply different potential causes. Inflammation, acute injury, and overuse are all big factors, but other factors to consider include anatomic anomalies (such as abnormal spine alignment, incases of scoliosis, or significant limb discrepancies). A thorough one-on-one diagnosis with a medical professional is the only way to ascertain (or rule out) piriformis syndrome, as well as other potential causes of back, leg, and buttock pain.
Managing and Reducing Piriformis Pain
If you have been diagnosed with piriformis syndrome, then it helps to know what can aggravate the situation, and why. Understanding that the piriformis is a muscle responsible for rotating and abducting the leg and hip can help – whenever you take long strides, walk up a step, spread your legs, or extend your hips, you are partially or fully contracting the piriformis.
Lying down and resting for too long, however, can also exacerbate the pain, because movement can help aid in recover and analgesia. Because the piriformis is involved in elementary everyday activities, it is almost impossible to give it a proper rest. Instead, try active recovery and a step back from intense movement. For example, consider:
-
- Reducing your activity level: Walking instead of running, taking the stairs at a slower pace with your other leg, switching to less intense physical exercise at the gym, etc.
- Taking anti-inflammatories: Ask your physician about safe over-the-counter painkiller use, and how often you should take NSAIDs if you are experiencing pain.
- Switching up your dietary habits: What you eat can affect your pain levels, especially if your diet tends to promote excessive inflammation. Making a few modest changes in what you eat could help you recover faster. General recommendations include eating more fish, more green vegetables, more fresh legumes, and fewer processed, canned, or refined foods.
- Mildly stretching your buttocks and hamstrings every day: In addition to continuing but slowing down your exercise regimen (or picking up a gentle exercise plan, to begin with), work with your physical therapist to pick out stretches and movements that help you relieve pain, and apply them every day. Some common examples include the Pigeon pose, thread-the-needle, and knee-to-chest stretches.
- Responsibly using hot-and-cold therapy: The evidence on cryotherapy and its effectiveness for muscle pain and inflammation is relatively lacking, but hot-and-cold therapies remain a common element of many pain management plans for muscle pains and strains. It’s important, however, to use these methods effectively to avoid adverse effects and complications, such as cold burns.
- Addressing contributing conditions: A foot problem, limb discrepancies, and spinal conditions can all indirectly or directly cause piriformis syndrome or contribute to its development and severity. Discussing, identifying, and treating underlying issues is an important part of the condition management process.
Piriformis syndrome is a condition that typically goes away on its own, as it tends to occur following injury or overuse. However, if the condition fails to go away, simply managing it through home remedies and exercise plans won’t be enough. Chronic piriformis syndrome requires more invasive treatment, ranging from corticosteroid injections or local anesthesia to reduce inflammation and pain, to surgery to address any long-term damage, and/or remove tissue.
Wallets, Cellphones and Back Pain
One of the most significant contributors to piriformis syndrome is sitting – but not just any kind of sitting. Aptly named “wallet neuritis”, prolonged periods of time spent with a large object compressing on the nerves in and around the buttocks can lead to neuropathy and inflammation, also known as peripheral sensitization (increased pain perception in the nerves outside of the brain and spine).
If you have made it a habit to sit with your wallet or phone in your back pocket, or sit on an unusually uncomfortable chair or stool, make arrangements to fix your sitting habits and get more ergonomic seating. It might save you from future pain, and help you recover quicker.
