Got Lumbar Spinal Stenosis? Stop Doing These 4 Things NOW
The human spine is a very strong collection of bones and tendons, supporting the body and the weight it carries for decades – until it doesn’t. Spinal conditions can often be debilitating, but their effects don’t have to be permanent. Yet one thing is clear: without a solid backbone, quality of life can drop fast.
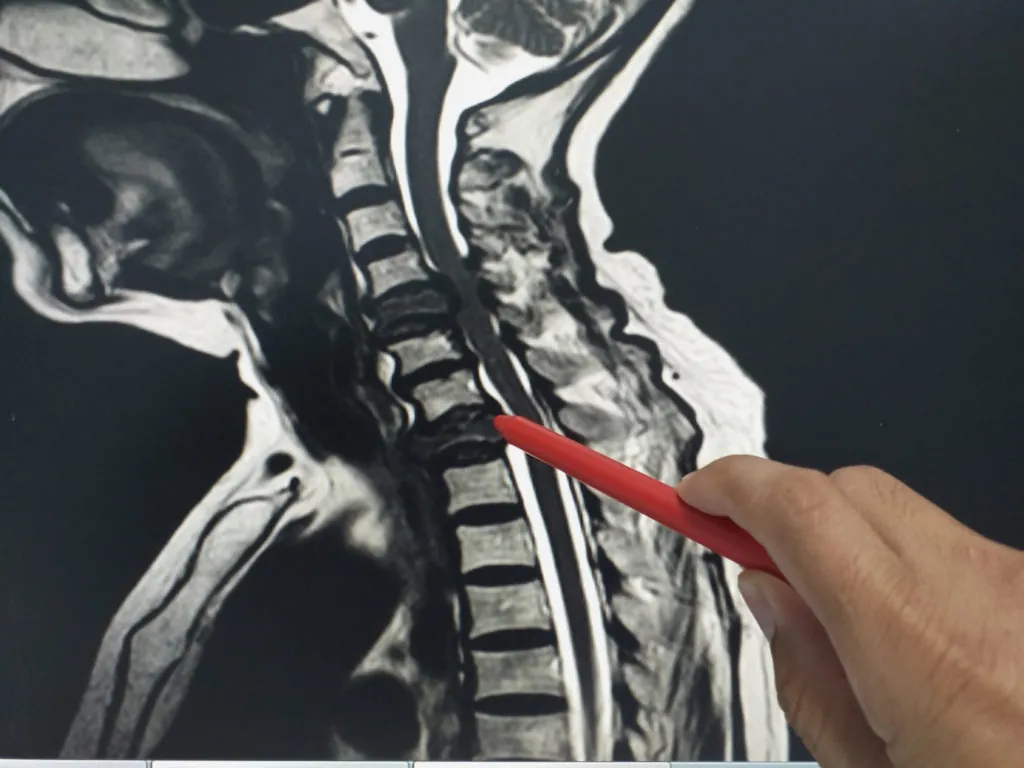
One such condition is spinal stenosis, or the narrowing of the spine causing damage to the spinal cord or surrounding nerves. When bony protrusions or cartilage between the vertebrae press on the spinal cord, the body reacts by experiencing numbness, loss of strength, difficulty controlling the bladder, and chronic pain.
There is no effective or safe cure for spinal stenosis – meaning, we cannot erase the damage it has done. But we can work to minimize it, help manage pain, and allow a patient with progressive spinal canal stenosis to maintain and even improve their condition. The key? Knowing not only what to do, but also what NOT to do.
Lumbar spinal stenosis is the most common form due to the lower back’s proclivity for injury, and the most common cause for spinal stenosis is age-related osteoarthritis – as the body ages, the bones weaken, and various factors lead to a condition wherein the spine potentially presses on its cord and surrounding nerves. If you have been diagnosed with lumbar spinal stenosis, these four tips are crucial:
1. Stop Doing Nothing
Spinal stenosis is not a condition that is improved simply through passive recovery. Though many other spinal issues resolve themselves if you simply give your body enough time and proper rest – including injury-induced sciatica – spinal stenosis is often a progressive issue, which means that if left unchecked, it will grow in intensity and the pain will worsen.
That means it’s important to take a proactive approach. While the narrowing of the spinal canal cannot be easily reversed, it can be slowed, and many treatments have shown promise in helping patients manage their pain, reduce inflammation, and improve both range of motion and quality of life.
Crucial to these improvements is an individualized and effective exercise regimen. The individualized portion here is important. It’s often not a good idea to grab a program off the internet because most exercise programs are heavily generalized to cater to a large group of people, even within a specific interest.
Because lumbar spinal stenosis can develop at different points throughout the lumbar region of the spine and for a myriad of reasons, any exercise program meant to effectively treat the pain and reduce both inflammation and pain would require the oversight and expertise of a trained physical therapist.
In the very least, meet with a professional physiotherapist, go through the motions to determine your current state, and receive advice on what movements and exercises to avoid, and which to prioritize.
2. Stop Relying on Medication
Prescription pain medications have their obvious drawbacks, with side effects ranging from decreased effectiveness in long-term treatment to full-blown addiction, yet even anti-inflammatory agents and acetaminophen (Tylenol/paracetamol) can cause the disease to progress at a more rapid pace.
The goal of anti-inflammatory medication is to reduce swelling and cause pain relief, which is a good thing in many circumstances – but it does not address the cause of the problem, nor does it help you maintain adequate range of motion and basic mobility.
This does not mean we advocate for any patient to drop all pain medication when treating their spinal stenosis. Instead, it is crucial to maintain awareness of the fact that medication alone will not do the trick.
Think of medication as a tool to further deal with the pain but think of corrective exercises and long-term physical therapy as key to slowing the pace of the condition and reducing the rate at which it is affecting your ability to move and live.
Anti-inflammatory medication can help patients recover from exercise and feel better after training, yet they should not be relied upon to mask the encroaching effects of spinal stenosis.
3. Stop Relying on a Handful of Exercises
To properly strengthen the muscles around the spine and slow the effects of osteoarthritis on your backbone, you must diversify your exercises. If you do not have regular contact with a physical therapist and instead choose to rely on programs online, then at least rely on core-strengthening exercises that are minimally dangerous to the lower back, and improve your ability to both flex the spine, and stretch the spine.
Many spinal stenosis exercise regimens focus on stretching the lower back to allow for the decompression of the spine, producing pain relief by elongating the spaces between the vertebrae and taking pressure off the spinal cord.
However, the condition can also be slowed by strengthening the lower back, taking pressure off the spine by building up the muscles around it. Slow and controlled back extensions on a glute-ham raise machine or on the floor, as well as weightless hip thrusts and other low-impact means of flexing the lower back (including stretches such as standing back extensions) can relieve pain and ensure that the muscles in and around the core are properly trained.
4. Stop Pushing for Surgery
Some of us have been taught to believe that when things get bad enough, only surgery can fix them. While that is often true, it isn’t always the case.
Research has shown that surgical intervention has netted minimal changes in patients with lumbar spinal stenosis, especially when compared to simple physical therapy and individualized training programs.
The difference between patients who underwent surgery and patients who opted for physical therapy in terms of long-term improvement were minimal – however, those who chose surgery had to deal with the potential for life-ending complications, ranging from infections to further inflammation and paralysis.
Treating Lumbar Spinal Stenosis
Lumbar spinal stenosis can occur due to age-related osteoarthritis, spinal injury, a past surgery, a tumor, or other forms of arthritis (including rheumatoid arthritis). Once it begins, it’s very hard to reverse, and no reliable cures currently exist.
However, by helping patients avoid posture mistakes and regularly train to strengthen their back, proper management of the condition can lead to a long-term delay of serious quality of life problems.
